- Topics
- Webinars
- Products & Services
- Customer Help
- Resources
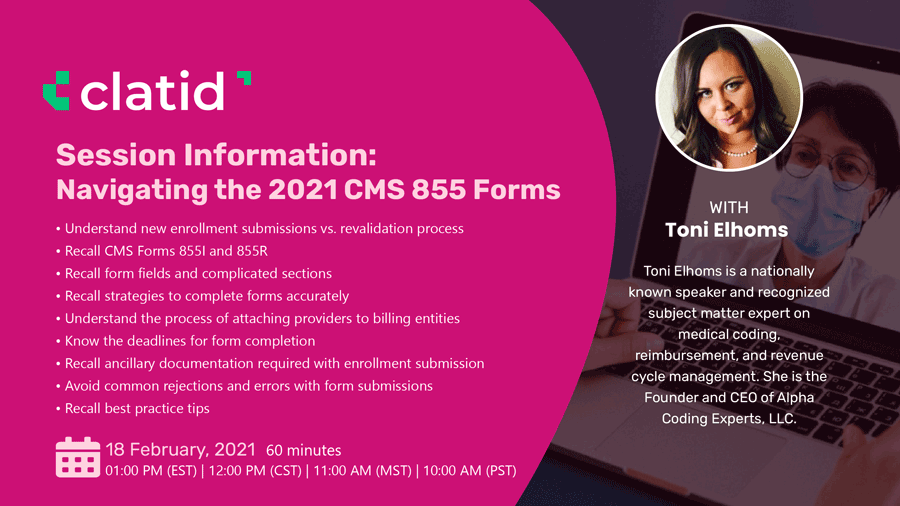
The process of enrolling with Medicare as a provider/organization can be tedious and time-consuming. The number of Medicare enrollment applications continues to decline due to the enormous complexities surrounding application submission. The cost of getting these enrollment application submissions wrong or missing a deadline can have systemic consequences on an organization, including credentialing issues, coding issues, denial issues, patient satisfaction, and even impact quality scores. During this information-packed webinar, Industry expert Toni Elhoms, CCS, CPS, CRC will discuss which providers are eligible for Medicare enrollment, the types of forms, how to navigate the form fillings, what ancillary documentation is needed with enrollment submission, applicable fees, common errors, and best practice tips.
-Discuss new enrollment submissions
-Discuss the revalidation process
-Review CMS Form 855I
-Review CMS Form 855R
-Discuss form fields and highlight complicate sections
-Discuss strategies to complete forms accurately
-The review process of attaching providers to billing entities
-Outline deadlines for form completions
-Outline ancillary documentation required with enrollment submission
-Discuss common rejections and errors with form submissions
-Discuss new enrollment submissions vs. revalidation process
-Review CMS Forms 855I and 855R
-Discuss form fields and highlight complicated sections
-Discuss strategies to complete forms accurately
-The review process of attaching providers to billing entities
-Outline deadlines for form completions
-Outline ancillary documentation required with enrollment submission
-Discuss common rejections and errors with form submissions
-Discuss best practice tips
-Understand new enrollment submissions vs. revalidation process
-Recall CMS Forms 855I and 855R
-Recall form fields and complicated sections
-Recall strategies to complete forms accurately
-Understand the process of attaching providers to billing entities
-Know the deadlines for form completion
-Recall ancillary documentation required with enrollment submission
-Avoid common rejections and errors with form submissions
-Recall best practice tips
-Credentialing professionals
-Practice managers
-Office managers
-Compliance professionals
-Billing professionals
-Coding professionals
-Contracting professionals
-Operations leadership

Toni Elhoms, CCS, CRC, CPC, AHIMA-Approved ICD10-CM/PCS Trainer is a nationally known speaker and recognized subject matter expert on medical coding, reimbursement, and revenue cycle management. She is the Founder and CEO of Alpha Coding Experts, LLC. She holds multiple credentials with the American Health Information Management Association (AHIMA) and the American Academy of Professional Coders (AAPC).
With over a decade of industry experience, she has led and supported hospital systems, universities, physician practices, payers, government agencies, and other entities on coding, billing, and compliance initiatives. She is a frequent contributor to various media outlets, speaker, and regular guest on industry podcasts. She created the Alpha Coding Podcast series to share her industry Pro-Tips. She also leads and mentors a network of revenue cycle management professionals across the country and serves as the President of the Orlando, FL AAPC Chapter.
Clatid Webinar Certification - Clatid rewards you with Clatid Achievement Certification for unlocking and attending this webinar. It is to acknowledge your participation in this training session and to add more to your professional score.
Clatid Courses and Webinar or any Education published "Articles & Materials" strictly follows the standards and guidelines of the Professional Credit / CEU Providers and Well Researched before publishment.
Clatid doesn't support any Fake - News, Articles, or Compliance updates; Our Industry Experts are highly verified and recognized, and their Pre-publishment is verified via our experts and fact-checkers.
Sign up now on clatid.io. Visit clatid.io/webinar to discover a wide range of webinars from industry specialists. Tick on either ‘live webinar’ or ‘on-demand’, and simply click on ‘buy now’ to get enrolled.
You can refer Clatid to anyone in your social circle. Explore your industry with your colleagues by getting them signed up on clatid.io today!
Go for the topic of your keen interest on clatid.io. Tick on ‘live webinar’ and get enrolled! Easy registration, transparent transaction.
You can request for an on-demand webinar that records the live webinar for you. After the webinar ends, you will have full access to the webinar’s recording. You can also explore Clatid offline to order your webinar DVDs, flash drives and transcripts.
If you can’t attend the live webinar, simply go for the ‘on-demand webinar’ for the same price! Now, the live webinar recording will be saved in a cloud storage for you to access anytime from anywhere.
Clatid offers both hard and soft copies of the webinars. It contains all the highlights as well as comprehensive descriptions of the webinar, so you never miss out a single detail.
After attending the live webinar, your certificate will be emailed to you. You can download it and add more charm to your professional score.
At the end of each webinar, you have the opportunity to interact with your industry experts, where you will get answers to all your queries.
Can’t attend the live webinar? Clatid has got you covered! You can always switch to the on-demand webinar from your portal. You can also get your hands on the webinar’s DVD/flash drive and transcript. So order them now!
Clatid brings a variety of options for offline learning. Order your DVDs, flash drives or transcripts now to have a lifetime access to Clatid webinars. You can also go for on-demand recordings. Download and watch it anytime from anywhere in the world!


